Introduction
Achieving and maintaining healthy skin is a priority for many individuals, but it can be challenging when faced with various skin conditions. Two commonly confused conditions are fungal acne and closed comedones. In this article, we will delve into the characteristics, causes, and treatment options for these two distinct skin concerns. also the Understanding the Differences: Fungal Acne vs Closed Comedones. By understanding the differences between fungal acne and closed comedones, you can better address and manage your skin concerns effectively.
Understanding Fungal Acne

Fungal acne, also known as pityrosporum folliculitis, is a common skin condition caused by an overgrowth of yeast on the skin. The yeast responsible for fungal acne is often a type called Malassezia, which naturally resides on the skin. However, certain factors can trigger its overgrowth, leading to the development of fungal acne.
Identifying fungal acne requires recognizing its distinct symptoms. This condition typically appears as tiny, uniform, red or skin-coloured bumps on the face, chest, or back. Unlike traditional acne, which can include various types of lesions, fungal acne lesions are usually similar in size and shape. They may also have a characteristic appearance of “clusters” or a rash-like pattern.
The texture of fungal acne can be slightly rough or bumpy, resembling small raised bumps. It is important to note that these bumps are not filled with pus like traditional acne. Instead, they are caused by inflammation in the hair follicles due to yeast overgrowth.
Factors contributing to the development of fungal acne include environmental conditions and personal habits. Hot and humid climates create a favourable environment for the proliferation of Malassezia yeast. Excessive sweating can also contribute to the development of fungal acne as sweat can mix with yeast on the skin. Wearing tight clothing or occlusive materials that trap heat and moisture can further exacerbate the condition. Additionally, the use of heavy, oil-based skincare products or prolonged use of antibiotics can disrupt the balance of the skin’s natural microbiome and encourage the growth of yeast.
Proper diagnosis of fungal acne is essential for accurate identification and effective treatment. While the symptoms may provide a strong indication, it is recommended to consult a dermatologist for a professional evaluation. A dermatologist can examine the affected areas and may perform additional tests, such as a skin scraping or culture, to confirm the presence of yeast.
In some cases, fungal acne may be mistaken for closed comedones or traditional acne. Closed comedones, as mentioned earlier, are clogged hair follicles beneath the skin’s surface. They typically appear as closed, white or flesh-colored bumps. Traditional acne, on the other hand, can include various types of lesions such as blackheads, whiteheads, papules, pustules, or cysts. Understanding the distinctions between these conditions is crucial to ensure appropriate treatment is administered.
Once fungal acne is diagnosed, treatment options can effectively target the underlying yeast overgrowth and reduce inflammation. Topical antifungal medications, such as ketoconazole or ciclopirox, are commonly prescribed to combat the overgrowth of yeast. These medications work by inhibiting the growth of yeast cells and reducing the associated inflammation. In some cases, oral antifungal medications may be necessary for severe or persistent fungal acne.
In addition to medication, adopting an appropriate skincare routine and practicing good hygiene are essential for managing and preventing fungal acne. Using gentle cleansers that do not strip the skin’s natural oils and avoiding heavy, occlusive products can help maintain a balanced skin environment. Incorporating antifungal agents, such as tea tree oil or pyrithione zinc, into the skincare routine can provide additional support in combating yeast overgrowth.
Dietary and lifestyle modifications may also complement traditional treatment methods for fungal acne. A diet rich in probiotics, such as yoghurt or fermented foods, can help promote a healthy balance of microorganisms on the skin. Antioxidant-rich foods, like fruits and vegetables, can support overall skin health and strengthen the body’s immune response. Regular exercise, stress management techniques, and adequate sleep can also contribute to overall well-being and skin health.
Remember, accurate diagnosis and personalized treatment guidance from a dermatologist are crucial for effectively managing fungal acne. They can provide tailored recommendations based on the severity of your condition, skin type, and specific needs.
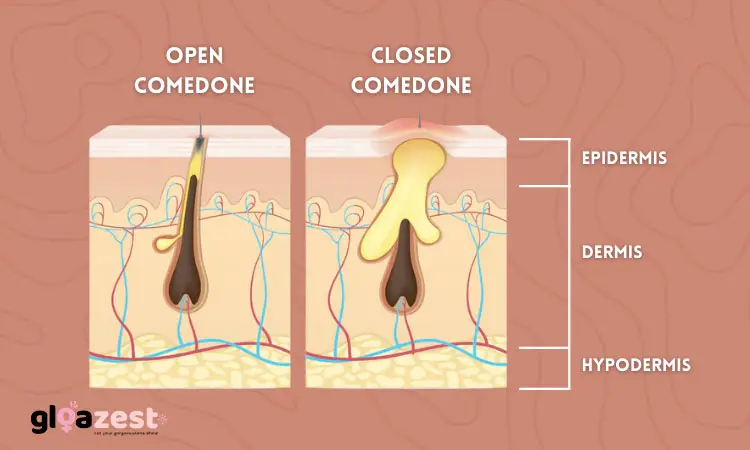
Closed Comedones: The Basics

Closed comedones, commonly known as whiteheads, are a form of acne characterized by clogged hair follicles beneath the skin’s surface. They occur when dead skin cells, oil, and bacteria accumulate and block the follicle opening, resulting in a closed, white or flesh-colored bump. Closed comedones are considered non-inflammatory acne lesions, meaning they do not usually cause redness or swelling.
These comedones are most commonly found on the face, particularly in areas with a high concentration of sebaceous glands, such as the forehead, nose, and chin. However, they can also occur on the chest, back, and other parts of the body.
Understanding the causes and risk factors associated with closed comedones can help in managing and preventing their occurrence. Excess oil production, also known as sebum, is a primary contributor to closed comedones. Hormonal changes, such as those during puberty, pregnancy, or menstrual cycles, can increase sebum production and make individuals more prone to developing closed comedones.
Certain skincare products can also play a role in the development of closed comedones. Using heavy, oil-based products or those that are not suitable for your skin type can contribute to clogged pores. Comedogenic ingredients, such as certain oils or silicones, can exacerbate the formation of closed comedones in susceptible individuals.
While closed comedones are non-inflammatory, they can become inflamed and evolve into other types of acne lesions if bacteria infect the clogged pore. This can lead to the development of papules, pustules, or cysts. It is important to avoid squeezing or picking at closed comedones to prevent further inflammation and potential scarring.
Differentiating closed comedones from other types of acne is essential for proper treatment. Open comedones, also known as blackheads, are similar to closed comedones but have an open pore, allowing the contents to oxidize and turn dark in color. Inflammatory acne lesions, such as papules, pustules, or nodules, are characterized by redness, swelling, and often pain or tenderness.
Treating closed comedones involves a multi-faceted approach to unclog the pores, reduce oil production, and prevent new comedones from forming. Topical treatments containing ingredients such as salicylic acid or benzoyl peroxide are commonly used to exfoliate the skin, remove dead cells, and reduce oiliness. These treatments can help unclog the pores and minimize the formation of new closed comedones.
It is important to introduce these treatments gradually to minimize potential skin irritation and dryness. Non-comedogenic skincare products, specifically formulated not to clog pores, should be used to prevent further comedone formation. Regular gentle cleansing, preferably with mild, non-abrasive cleansers, can help remove excess oil and impurities from the skin’s surface.
In some cases, professional extraction of closed comedones may be necessary. Dermatologists or licensed estheticians can perform this procedure using specialized tools to gently remove the contents of the comedones without causing damage to the skin.
Preventing closed comedones involves adopting a consistent skincare routine and making certain lifestyle adjustments. Regularly cleansing the skin, avoiding heavy or occlusive products, and using non-comedogenic moisturizers and sunscreens can help maintain clear pores. Additionally, maintaining a balanced diet, managing stress levels, and avoiding habits that worsen acne, such as excessive touching or picking at the skin, can contribute to the prevention of closed comedones.
Remember, if closed comedones persist or worsen despite appropriate skin care measures, it is advisable to consult a dermatologist. They can provide personalized recommendations and treatments based on the severity and individual characteristics of your skin condition.
Fungal Acne vs. Closed Comedones: Key Differences
When comparing fungal acne and closed comedones, several key differences stand out. Firstly, their physical appearance and texture vary significantly. Fungal acne presents as small, red or skin-coloured bumps with a slightly rough texture, while closed comedones appear as closed, white or flesh-colored bumps that are usually smooth.
The localization and distribution of these two conditions also differ. Fungal acne tends to affect areas with a higher density of sweat glands, such as the forehead, upper back, and chest. In contrast, closed comedones predominantly appear on the face, particularly in the T-zone, which encompasses the forehead, nose, and chin.
Furthermore, the underlying causes and contributing factors of fungal acne and closed comedones are distinct. Fungal acne arises from an overgrowth of yeast on the skin, often triggered by factors such as hot and humid climates, excessive sweating, or the use of occlusive skincare products. On the other hand, closed comedones are primarily caused by the accumulation of dead skin cells, oil, and bacteria within the hair follicles, influenced by hormonal imbalances and the use of comedogenic products.
Additionally, the secondary symptoms and associated conditions can aid in distinguishing between fungal acne and closed comedones. Fungal acne may be accompanied by itchiness, discomfort, or a “yeasty” smell, whereas closed comedones typically do not cause any itching or discomfort unless they become inflamed or infected.
10 key differences between fungal acne vs closed comedones
| Fungal Acne | Closed Comedones |
|---|---|
| Caused by yeast overgrowth | Caused by clogged hair follicles |
| Appears as red or skin-colored bumps with a slightly rough texture | Appears as closed, white or flesh-colored bumps that are usually smooth |
| Commonly found on the forehead, chest, and back | Predominantly occurs on the face, particularly in the T-zone (forehead, nose, and chin) |
| Can be itchy or uncomfortable | Typically does not cause itching or discomfort |
| Often clusters in specific areas | Can appear in various areas on the face |
| Associated with a “yeasty” smell | Does not have a distinct smell |
| Diagnosis requires examination by a dermatologist or medical professional | Diagnosis can often be made based on visual appearance |
| Requires specific antifungal treatment | Can be treated with topical treatments such as salicylic acid or benzoyl peroxide |
| Aggravated by hot and humid climates, excessive sweating, or occlusive skincare products | Influenced by excess oil production, hormonal changes, and comedogenic skincare products |
| May be accompanied by additional symptoms such as rash or redness | Typically does not have additional associated symptoms |
Treatment Options for Fungal Acne

When it comes to treating fungal acne, the primary approach involves the use of antifungal medications. Topical treatments containing antifungal agents, such as ketoconazole or ciclopirox, can effectively target and eliminate the overgrowth of yeast. These medications are usually available over the counter or can be prescribed by a dermatologist.
In addition to topical antifungal medications, adopting an appropriate skincare routine and practising good hygiene are essential for managing and preventing fungal acne. Use gentle cleansers and avoid heavy, occlusive products that can contribute to yeast overgrowth. Incorporating antifungal agents into your routine, such as tea tree oil or pyrithione zinc, can also provide additional support.
Dietary and lifestyle modifications may complement traditional treatment methods for fungal acne. A diet rich in probiotics and antioxidants, along with regular exercise and stress management techniques, can contribute to overall skin health and reduce the likelihood of fungal acne flare-ups.
Managing and Preventing Closed Comedones
Topical treatments play a significant role in managing closed comedones. Look for products containing ingredients like salicylic acid or benzoyl peroxide, which help exfoliate dead skin cells, reduce inflammation, and unclog pores. It’s essential to introduce these treatments gradually to prevent excessive dryness or irritation.
Incorporating gentle exfoliation and proper cleansing techniques can aid in managing closed comedones without causing further irritation. Exfoliating with mild chemical exfoliants, such as alpha-hydroxy acids (AHAs) or beta-hydroxy acids (BHAs), helps remove dead skin cells and prevent pore blockages. Remember to moisturize adequately to maintain a balanced skin barrier.
Choosing non-comedogenic skincare products is crucial to prevent the formation of closed comedones. Non-comedogenic products are formulated to avoid clogging pores, reducing the likelihood of comedone development. Read product labels carefully and opt for oil-free or water-based formulas.
Lifestyle factors, such as stress and diet, can also influence the occurrence and severity of closed comedones. Minimize stress levels through relaxation techniques or activities you enjoy. Additionally, incorporating a balanced diet rich in fruits, vegetables, and whole grains while limiting processed foods and sugary snacks can promote overall skin health.
Conclusion of Fungal Acne vs Closed Comedones
In conclusion, understanding the differences between fungal acne vs closed comedones is essential for accurate diagnosis and effective treatment. Fungal acne is caused by an overgrowth of yeast, while closed comedones result from clogged hair follicles. Recognizing the distinctive characteristics, causes, and associated symptoms of these conditions is vital for choosing appropriate treatment options.
If you are experiencing skin concerns, it is always recommended to consult a dermatologist for personalized advice and treatment. They can accurately diagnose your condition and provide tailored recommendations to address your specific needs. Remember, taking proactive steps in your skincare routine, maintaining proper hygiene, and adopting a healthy lifestyle can significantly contribute to healthier skin.
FAQs
Q1: Can fungal acne and closed comedones occur simultaneously?
A1: Yes, it is possible to have both fungal acne and closed comedones simultaneously. Each condition requires specific treatment approaches, so it is essential to consult a dermatologist for an accurate diagnosis and personalized treatment plan.
Q2: Can I treat fungal acne with traditional acne treatments?
A2: Traditional acne treatments, such as benzoyl peroxide or salicylic acid, are not effective against fungal acne. Fungal acne requires antifungal treatments specifically designed to target the overgrowth of yeast. Consult with a dermatologist to ensure appropriate treatment.
Q3: Are closed comedones contagious?
A3: No, closed comedones are not contagious. They are a result of internal factors, such as excess oil production and dead skin cell buildup. However, bacteria can infect closed comedones, leading to inflammation and possible breakouts. Maintaining proper skincare and hygiene practices can help prevent such infections.
Q4: Can diet influence the occurrence of closed comedones?
A4: While diet alone may not directly cause closed comedones, certain dietary factors can influence their occurrence. Research suggests that diets high in refined carbohydrates and processed foods may contribute to increased sebum production and inflammation, both of which can exacerbate the formation of closed comedones. On the other hand, diets rich in fruits, vegetables, and foods containing essential fatty acids may promote skin health and reduce the likelihood of developing closed comedones. It’s important to maintain a balanced diet and incorporate nutritious foods for overall skin health.
Q5: Can closed comedones be popped or squeezed?
A5: It is generally not recommended to pop or squeeze closed comedones. Applying pressure to these bumps can lead to further inflammation, infection, and scarring. Moreover, forcibly extracting the contents of a closed comedone may not effectively remove the underlying clog, and the comedone may reoccur. If you are concerned about closed comedones, it is best to consult a dermatologist who can provide appropriate extraction techniques or recommend suitable treatments.
Q6: Can closed comedones be prevented?
A6: While it may not be possible to completely prevent closed comedones, adopting certain skincare practices can help minimize their occurrence. Regularly cleansing your skin with a gentle cleanser can remove excess oil and impurities that can contribute to clogged pores. Exfoliating with gentle chemical exfoliants, like AHAs or BHAs, can help prevent dead skin cell buildup. Additionally, using non-comedogenic skincare products and avoiding heavy, pore-clogging ingredients can reduce the risk of closed comedone formation.
Q7: How long does it take to see results with treatment for fungal acne or closed comedones?
A7: The timeline for seeing results with treatment can vary depending on several factors, including the severity of the condition, the chosen treatment approach, and individual skin response. In general, it may take several weeks to a few months of consistent treatment before significant improvements are noticeable. It is important to follow the recommended treatment regimen and be patient throughout the process. If you do not see improvements or if your condition worsens, it is advisable to consult a dermatologist for further guidance.
Q8: Can hormonal changes contribute to the development of closed comedones?
A8: Hormonal changes can indeed play a role in the development of closed comedones. Fluctuations in hormone levels, particularly during puberty, menstruation, or hormonal imbalances, can stimulate increased sebum production. This excess sebum can mix with dead skin cells and bacteria, leading to the formation of closed comedones. Understanding the hormonal factors contributing to your skin condition can help guide treatment approaches and management strategies.


Leave a Reply